Minimally Traumatic Stapes Surgery
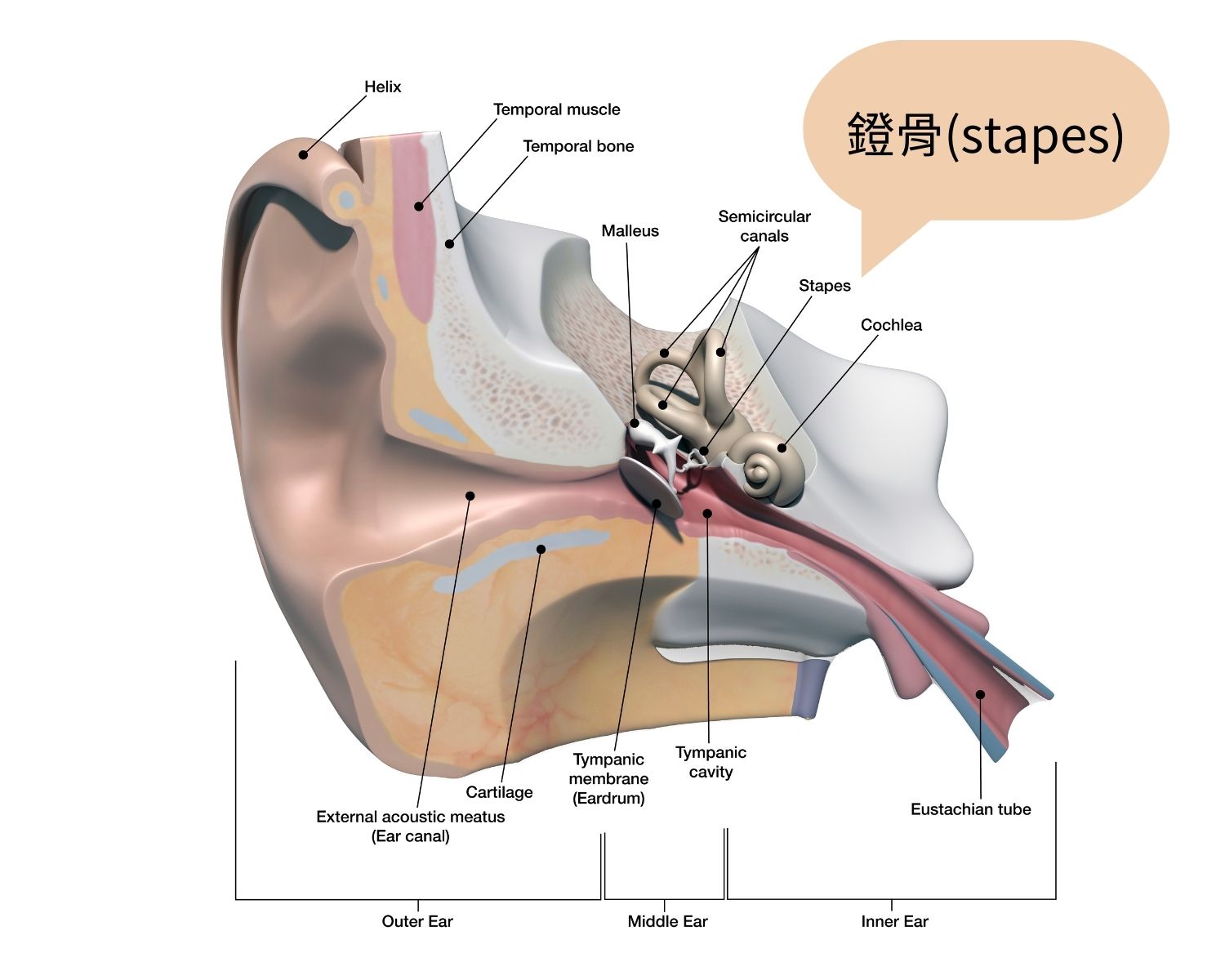
Minimally traumatic stapes surgery is a surgical procedure used to treat otosclerosis, also known as “abnormal hardening of ossicles”, which can lead to hearing loss when the stapes becomes hardened and cannot transmit sound waves properly to the inner ear. Unlike elderly individuals, young people should be aware if hearing decline is noted. In addition to common causes such as acute eardrum perforation or inflammation, a professional examination and evaluation is necessary to confirm a diagnosis of otosclerosis. Normal hearing depends on the transmission of sound waves through the ear canal, which are amplified by the ossicles: the malleus, incus, and stapes. The stapes is the smallest of these bones and is responsible for transmitting sound waves to the inner ear. When the stapes becomes hardened and unable to transmit sound, the only solution is surgical treatment of this small, rice-sized bone.
Dr. Shiao An-Suey, the Director of the Department of Otolaryngology at Cheng Hsin General Hospital in Taiwan, is an authority in the treatment of otosclerosis. He not only has the highest surgical success rate in Taiwan, but also developed the minimally traumatic stapes surgery. This new surgical technique decreases many postoperative complications including persistent vertigo and worsening of hearing and allows patients to rapidly restore hearing within one to two months.
The surgical procedure firstly involves stabilizing the patient’s position. Within the middle ear, drill a small hole on the footplate of the ossified stapes and insert a piston-like implant to replace the function of the ossified stapes. The ossified stapes is then removed. The remaining ear canal space is packed with gelform. It is worth noting that special care must be taken during every steps of procedures especially avoid damaging the inner ear’s oval window. If the floating footplate accidentally fall into the inner hear during surgery, it could result in postoperative vertigo and hearing loss.
Furthermore, chorda tympani nerve which are responsible for taste locates closely to the auditory ossicles. If injured, the patient may experience temporary taste alterations. Fortunately, this typically returns to normal as recovery progresses within one to two months after the surgery.
Patients who undergo minimally traumatic stapes surgery could expect a faster recovery. In the early postoperative period, patients should avoid lifting heavy objects, diving, or blowing their nose excessively to reduce the pressure in the middle ear. However, there are usually no restrictions on air travel for the general public. Follow-up appointments will be scheduled several times within two months after the surgery. Dr. Shiao An-Suey pointed out that otosclerosis is common in white people in Europe and America, but rare in Asians. Its occurrence is closely related to genetics, and hormonal changes may also contribute. As many as 70% to 80% of patients only experience in one ear. Differential diagnosis of otosclerosis is critical. In addition to history of gradual hearing loss, it is essential to rule out whether the patient has had inflammation inside the ear or a congenital problem.
Dr. Shiao An-Suey emphasized the importance of comprehensive evaluation before operation. Pure-tone audiometry and assistive hearing tests will be arranged for patients in clinical practice. Computed tomography scans of inner ear without contrast can also identify other problems within the ear.
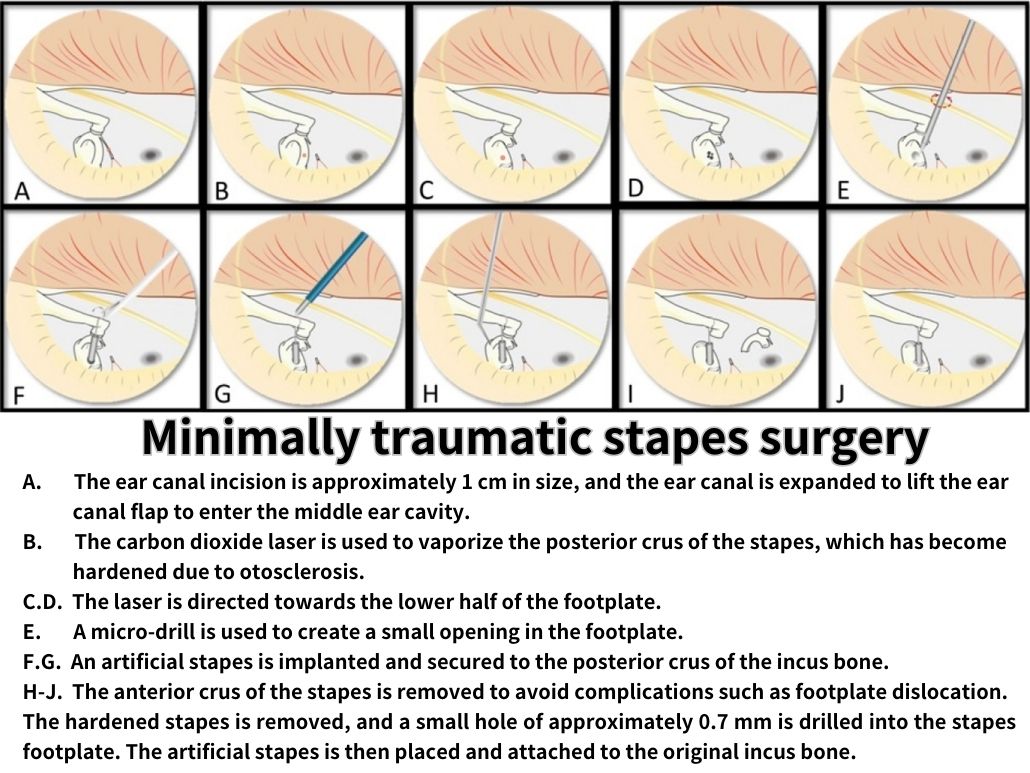
Generally, if the air-bone gap (ABG) is greater than 20dB which causing significant hearing difference, surgery may be recommended for the patient. However, if the ABG is lower than standard or the patient is over 65 years old, surgery is not recommended. The stapes, which is located in the middle ear, is almost the size of a grain of rice. Stapedotomy surgery to treat otosclerosis is an extremely delicate and high-difficulty microsurgery. The surgeon must have excellent skills and use a large microscope with magnification of 20 times or more to complete the endoscopic surgery within 1 to 1.5 hours in the ear canal, which is only about 1 cm in reality.
Currently, the average global success rate of stapes surgery ranges from 60-90%. Dr. Shiao An-Suey, the Director of the Department of Otolaryngology at the Cheng Hsin General Hospital, has achieved a success rate of over 90% through over a decade of continuous research and development. His innovative “minimally invasive stapes surgery” technique has significantly decreased postoperative complications such as vertigo, inflammation and hearing deterioration.
Dr. Shiao has become a World-Class surgeron in his field. Although each individual may have varied perspective and requirement of hearing, Dr. Shiao emphasizes that relying on single-ear hearing can result in lack of stereoscopic sense and inability to identify acoustic spatial, which can impact daily life. Minimally invasive stapes surgery has now evolved into a safe and effective ear surgery, and it is the only permanent solution for otosclerosis.

An-Suey Shiao, Head of Department
Position
Director, Department of Otolaryngology, Cheng Hsin General Hospital
Education
- 1972-1979 M.D. National Defense Medical Center
- 1990 Fellowship, Cincinnati Children Hospital, U.S.A.
- 1990 Fellowship, Pittsburg Children Hospital, U.S.A.
Specialization
- Otosclerosis surgery (Taiwan first)
- Otitis media and cholesteatoma surgery (SNQ National Biotechnology Medical Quality Bronze Medal)
- Cochlear implantation (study in Australia)
- Diagnosis and treatment of dizziness, tinnitus and hearing impairment
- Diagnosis and treatment of pediatric otolaryngology patients (to study in the United States)
- Hearing energy rehabilitation and hearing aid selection




 Mon~ Fri 8am~5pm.
Mon~ Fri 8am~5pm.


